
Standardisation and Globalisation
As Traditional Chinese Medicine enters the digital age, standardisation and global integration have become essential for its continued relevance and credibility. Integrating AI into TCM diagnosis—while offering remarkable advances in objectivity and precision—demands the development of clear, uniform data collection, interpretation, and clinical application protocols.
To achieve consistency across practices, it is critical to establish standardised diagnostic frameworks, terminologies, and performance metrics that define how pulse, tongue, facial, auditory, and olfactory data are measured, analysed, and interpreted. These frameworks must honour the integrity of TCM’s holistic principles and align with the rigorous expectations of scientific and technological systems.
Establishing international standards, such as those supported by the International Organisation for Standardisation (ISO) and the World Health Organisation (WHO), will play a central role in this transformation. These global benchmarks will help ensure:
-
Quality and safety in AI-driven diagnostics
-
Reproducibility and reliability across clinical settings
-
Interoperability between digital diagnostic platforms and medical devices
-
Global collaboration in research, training, and clinical implementation
Standardisation will also lay the foundation for regulatory approval and institutional adoption of TCM diagnostic technologies in healthcare systems worldwide. As a result, AI-enhanced TCM will gain greater recognition within evidence-based medicine and contribute meaningfully to the broader movement toward integrative and personalised healthcare.
Ultimately, the globalisation of TCM—powered by standardised, AI-supported diagnostic systems—offers a future where ancient wisdom and cutting-edge innovation coexist. Building a common language between tradition and technology and across nations and cultures can unlock TCM's full potential to promote health, healing, and harmony worldwide.
AI Assisted Tongue Reading
Enhanced by artificial intelligence and computer vision advancements, AI-analysed tongue diagnosis is revolutionising one of Traditional Chinese Medicine’s (TCM) most ancient and intuitive diagnostic techniques. By automating the interpretation of tongue features, these systems help identify patterns that correlate with internal imbalances in Qi, blood, and organ systems, thus supporting practitioners with faster, more standardised assessments. AI-analysed tongue reading is a computer-aided diagnostic system that interprets tongue images using TCM diagnostic principles. The system uses machine learning algorithms—particularly convolutional neural networks (CNNs)—to assess key visual features and map them to recognised TCM syndromes. The Five Phases of AI-analysed tongue reading include:
-
Image Capture: The process begins with the user or patient taking a high-resolution image of their tongue using a smartphone or specialised diagnostic device. To ensure diagnostic reliability, guidelines are followed for lighting (preferably standardised or natural white light), angle (tongue flat, fully extended), tongue position and background (neutral, non-reflective)
-
Image Preprocessing: Before analysis, the image undergoes preprocessing to enhance clarity and isolate relevant regions background removal and noise reduction lighting correction and colour normalisation and the segmentation of the tongue into standard diagnostic zones (e.g. tip (Heart), sides (Liver and Gallbladder), centre (Spleen and Stomach) and root (Kidney, Bladder, Intestines))
-
Feature Assessment: The AI uses trained computer vision algorithms to evaluate the tongue’s surface for features significant in TCM.
-
Pattern Matching: Once features are extracted, the system compares them to a library of labelled images and diagnostic case data. The AI then matches the user’s tongue characteristics to known TCM syndrome patterns such as Spleen Qi Deficiency with Damp, Liver Fire Rising, Heart Yin Deficiency or Blood Stagnation with Internal Cold
-
Diagnostic Report Generation: The final phase is the creation of a comprehensive diagnostic report, which may include a summary diagnosis (e.g., “Mild Qi and Blood Deficiency with Damp Accumulation”), a tongue map highlighting affected zones and linked organ systems, tailored recommendations based on the syndrome identified:, suggestions for herbal formulas, acupuncture points, dietary and lifestyle modifications and a prompt to consult with a licensed TCM practitioner for deeper evaluation
AI-assisted tongue reading systems promise to transform TCM diagnosis by introducing objectivity, reproducibility, and standardisation. By training these algorithms on large, diverse datasets—with expert-annotated labels and diagnostic histories—AI can detect subtle visual patterns that may elude the human eye. Over time, these systems will evolve to reduce practitioner subjectivity, improve diagnostic accuracy across varied populations, enable early detection of imbalances and integrate with telemedicine platforms for remote diagnosis and self-care.
Although challenges remain—particularly in achieving standardised image conditions, colour calibration, and clinical validation—the pathway toward reliable AI-driven tongue diagnosis is becoming increasingly clear. As Matos et al. (2021) noted, improvements in imaging technology combined with advanced data processing will contribute significantly to overcoming current limitations and accelerating the modernisation of tongue diagnosis in clinical practice.



To overcome the inherent variability of traditional pulse readings, AI algorithms are employed to preprocess pulse data, including filtering, denoising, and normalisation, to ensure signal clarity and consistency. These preprocessing steps are critical for transforming raw tactile signals into data suitable for accurate interpretation and classification.
One of the current challenges in the field is the lack of cross-device compatibility. Different pulse measurement devices, developed by various manufacturers, may vary in sensor type, data format, and sensitivity. AI technologies are now designed to enhance interoperability, allowing algorithms to interpret data consistently across multiple platforms. This effort is key to achieving data standardisation for clinical reliability and large-scale adoption. However, AI-driven pulse diagnosis in TCM still faces limitations due to the absence of universally accepted diagnostic standards and the slow development of robust, standardised measurement devices. Without uniform benchmarks for pulse characteristics and diagnostic criteria, validating and scaling these technologies in clinical settings is difficult.
To address these gaps, the future development of pulse measurement systems must focus on establishing unified pulse data protocols, promoting inter-device data compatibility, and integrating multiple diagnostic modalities (e.g., tongue, facial analysis, and pulse) into comprehensive AI platforms and conducting clinical validation studies to align machine-generated insights with practitioner expertise.
The Quantification of Pulse Diagnosis
The quantification of pulse patterns is critical in transforming Traditional Chinese Medicine (TCM) pulse diagnosis from a subjective art into a standardised, evidence-based clinical tool. Traditionally, pulse diagnosis depends on a practitioner’s tactile sensitivity and interpretive skill to distinguish between complex pulse types, such as wiry, slippery, thready, or deep pulses, each corresponding to distinct internal conditions. However, this process is inherently subjective, lacking consistent parameters or measurable data that can be reliably shared, reproduced, or validated across practitioners and settings.
AI-directed pulse diagnosis focuses on systematically quantifying pulse signals through high-resolution sensors and advanced data analytics to address this limitation. These systems capture and digitise arterial pulse waveforms, enabling the extraction of a wide range of quantifiable features, including:
-
Amplitude and intensity
-
Pulse waveform shape.
-
Wavelength and frequency
-
Peak intervals and ratios
-
Phase differences
-
Pulse depth and duration.
-
Rate variability and rhythm regularity.
Once these variables are extracted, AI algorithms—particularly deep learning models such as convolutional neural networks (CNNs) or recurrent neural networks (RNNs)—are trained on labelled datasets to recognise and classify patterns corresponding to traditional TCM pulse types. These models can emulate practitioner interpretation while reducing human error and bias.
Quantification also allows for data consistency across different devices and users, longitudinal monitoring of patient conditions, comparative studies across populations, treatment protocols, and geographic regions and multimodal integration with other diagnostic streams (e.g., tongue and face analysis) for holistic syndrome differentiation. However, realising the full potential of AI-directed pulse diagnosis requires the development of standardised diagnostic criteria and uniform data acquisition protocols. Without agreed-upon definitions for pulse features or benchmark datasets, there is a risk of fragmentation and inconsistent clinical outcomes. Thus, ongoing research efforts are focused on establishing universal pulse feature taxonomies, creating large-scale, annotated datasets based on practitioner-labelled cases, enhancing signal fidelity and sensor resolution and integrating AI models into user-friendly platforms for clinical and home-based applications.
Quantifying pulse patterns through AI enhances diagnostic precision and lays the groundwork for the scientific modernisation of TCM. As AI continues to evolve, its role in standardising and scaling pulse diagnosis will be central to building trustworthy, data-driven, and globally accessible TCM diagnostic systems.

TCM Dianostics
Traditional Chinese Medicine (TCM) diagnosis is grounded in a holistic worldview that sees the human body as an integrated system of physical, emotional, and energetic functions constantly interacting with the environment. Rather than isolating symptoms or relying solely on molecular markers and physiological indicators, TCM aims to assess the totality of an individual’s health, considering both internal imbalances and external influences. Diagnosis is not about identifying a disease in isolation but about understanding patterns of disharmony and their root causes to guide personalised and dynamic treatment strategies. Central to this diagnostic framework are the Four Diagnostic Methods:
-
Inspection (望, Wàng): Visual observation of the patient’s physical appearance, including complexion, posture, body shape, and tongue characteristics. This provides key indicators of internal organ function and systemic balance.
-
Auscultation and Olfaction (闻, Wén): Listening to the quality of the voice, breathing, and cough, and detecting odours from the body or breath to gather insights into internal pathologies.
-
Inquiry (问, Wèn): A comprehensive patient interview covering physical symptoms, emotional states, sleep, digestion, energy levels, menstruation (if applicable), diet, lifestyle, and medical history. This helps contextualise the observed symptoms and detect deeper imbalances.
-
Palpation (切, Qiè): Primarily pulse diagnosis, where practitioners feel the radial artery at three positions on each wrist (cun, guan, chi) and at varying depths to assess the condition of internal organs and energetic flow.
These diagnostic approaches allow the practitioner to identify patterns (or “syndromes”) rather than merely diagnose diseases. Each pattern reflects a specific constellation of signs and symptoms that point to underlying disharmonies in Qi, Blood, Yin-Yang balance, or organ function.
With the rise of Artificial Intelligence (AI), TCM is entering a new era where traditional methods are being digitised, standardised, and enhanced through cutting-edge technology. AI provides a promising pathway to overcome some of the historical challenges of TCM diagnostics, such as subjectivity, practitioner variability, and the lack of standardisation, by applying advanced sensors, machine learning algorithms, and data analytics to replicate and expand upon traditional diagnostic techniques.

AI-Assisted Diagnostics
Tactile sensors that simulate fingertip pressure to analyse pulse waveforms
02
High-resolution imaging and computer vision to perform detailed tongue and facial analysis.
01
03
Tactile sensors that simulate fingertip pressure to analyse pulse waveforms
Multimodal data integration platforms that consolidate inputs from inspection, palpation, inquiry, and auscultation into unified diagnostic models
05
Olfactory sensors and sound analysis to assist with smell and voice diagnostics.
04
AI Pulse Diagnosis
In Traditional Chinese Medicine (TCM), the pulse (mo) is regarded as one of the most important and sophisticated diagnostic techniques. It offers profound insights into the state of the patient’s internal organs and the flow of essential substances such as Qi (vital energy), Xue (blood), and body fluids. Mastering pulse diagnosis requires deep theoretical knowledge, highly developed tactile sensitivity, and diagnostic intuition.
Each of these three positions is palpated at three depths, which correspond to different physiological layers: the superficial level reflects Yang aspects and the condition of Qi, the intermediate level provides insight into blood and functional organ activity, and the deep level corresponds to Yin aspects, such as constitutional strength and the state of the Zang organs. These positions are further associated with the Three Burners (San Jiao) and cosmological principles.
Because of its complexity and subjectivity, pulse diagnosis demands years of hands-on training and clinical experience. Factors such as pulse depth, speed, strength, rhythm, width, and tension are evaluated simultaneously to identify one or more of the 28 traditional pulse types, each associated with specific patterns of disharmony.



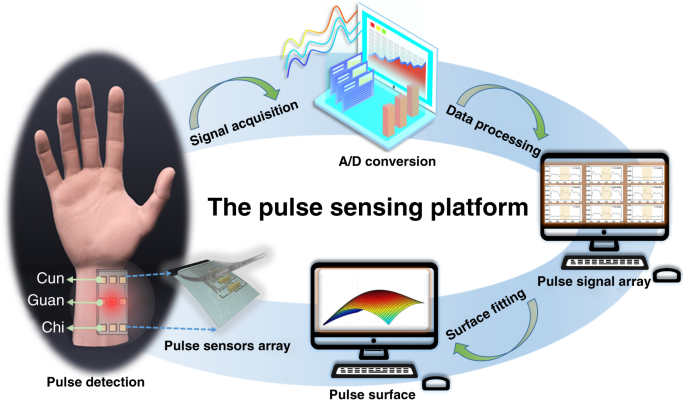
Arterial Pulse Waveform
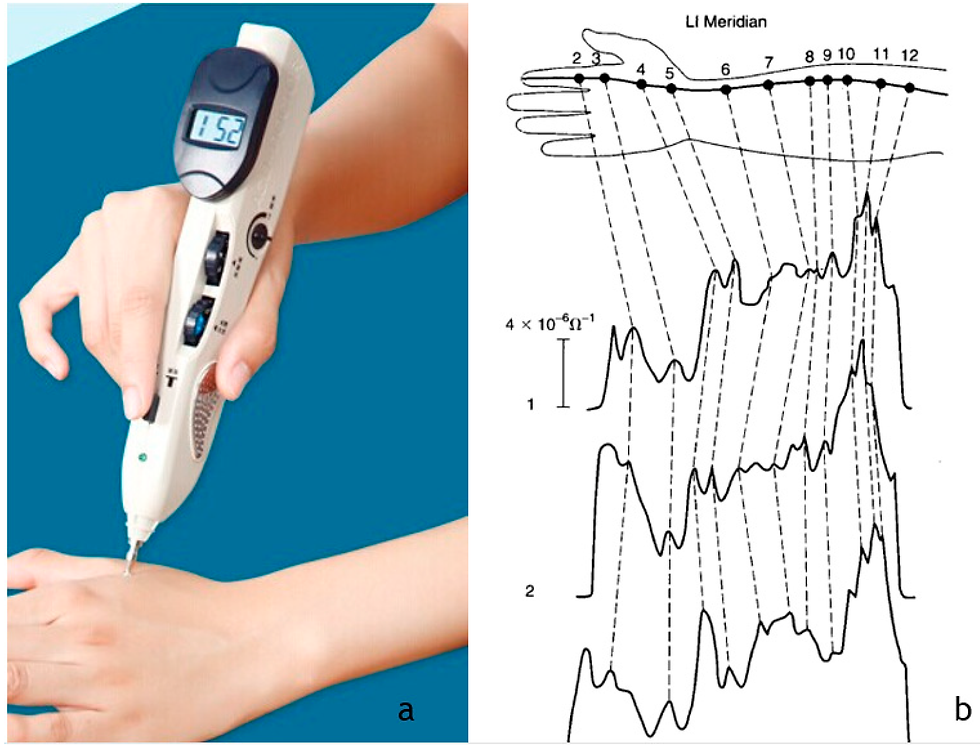
To modernise and standardise pulse diagnosis in Traditional Chinese Medicine (TCM), researchers have increasingly turned to the study of arterial pulse waveforms. This approach aims to develop objective, quantifiable strategies that can reflect traditional diagnostic categories with scientific precision. In pursuit of this goal, a wide variety of sensors have been employed to detect and capture pulse signals, including:
-
Piezoelectric sensors
-
Piezoresistive strain gauges
-
Magnetic and liquid sensors
-
Acoustic and Doppler ultrasonic devices
-
Infrared and optical photoelectric sensors
These technologies can translate tactile pulse sensations into digital waveforms, which can then be processed and analysed.
Once the pulse signal is acquired, it undergoes a series of computational steps to extract meaningful diagnostic information. Key waveform parameters include:
-
Wavelength
-
Relative phase difference
-
Rate parameters
-
Peak ratios
The relative variation between these indices serves as a basis for distinguishing between different pulse types, such as wiry, slippery, thready, or rapid, each associated with specific TCM syndromes. Researchers have begun integrating artificial intelligence (AI) techniques, particularly neural networks, to enhance diagnostic accuracy further and classify pulse patterns. Training these models on annotated pulse waveform datasets makes it possible to automatically recognise subtle distinctions between pulse qualities, thereby reducing practitioner subjectivity and advancing the goal of a standardised, objective pulse diagnosis system.
Pulse measurement devices represent a convergence of Traditional Chinese Medicine (TCM) diagnostic principles and modern technological advancements. These devices aim to enhance diagnostic accuracy, support personalised treatment plans, and improve patient engagement by making TCM pulse diagnosis more objective, measurable, and accessible. Options available on the pulse measurement device market include:
Pulse Measurement Devices
Combines AI-driven analysis with TCM and Ayurvedic principles to provide comprehensive health assessments. It evaluates organ energy levels, identifies root causes of health issues, offers diet and lifestyle recommendations based on pulse analysis, and generates detailed health reports with visualisations for better patient understanding.
1
An AI-powered device that blends ancient Ayurvedic wisdom with modern technology for precise health insights. It conducts comprehensive pulse readings in just 30 seconds, provides detailed reports on dosha balance, digestion efficiency, and organ energy levels and syncs with a dedicated mobile application for patient record management and progress tracking.
2
A multifunctional hardware and software complex designed for practitioners of traditional healing systems, including TCM. It evaluates functional health states using heart rate variability (HRV) analysis, creates personalised rehabilitation programs based on TCM principles, and offers modules for diet therapy, herbal recommendations, and more.
VedaPulse
2
A wearable device that uses airbags for pressurisation to collect pulse data, aligning with TCM diagnostic methods. It adjusts to locate Cun, Guan, and Chi regions on the wrist, captures pulse waveforms under varying pressures for comprehensive analysis and is suitable for home, medical, and experimental research applications.
1
A digital protocol for TCM pulse information collection using bionic equipment to ensure high efficiency and data integrity. It simulates traditional pulse-taking methods with robotic precision, generates rich pulse information, including multi-gradient dynamic pulse force time series and facilitates the standardisation of digitalised pulse information collection.
2
Tactile Array and Pulse Sensors
Tactile array technologies and pulse sensors have been successfully applied to detect specific arterial pulse characteristics, offering a more objective and replicable approach to Traditional Chinese Medicine (TCM) pulse diagnosis. Among the most advanced systems developed is the Bi-Sensing Pulse Diagnosis Instrument, which integrates a Pressure Displacement Bi-Sensing System with a robotic finger equipped with extremely sensitive pressure sensors.
These sensors are designed to simulate the tactile sensations of a TCM practitioner’s fingertips, capturing subtle variations in pulse depth, strength, and rhythm. The robotic fingers apply consistent, calibrated pressure across the wrist's Cun, Guan, and Chi positions, producing high-resolution pulse waveforms.
Studies have shown that the pulse signals acquired from these robotic systems closely match the diagnostic impressions of skilled TCM practitioners, demonstrating their potential as effective tools for standardising pulse diagnosis and supporting clinical decision-making. By combining tactile sensing with AI-driven pattern recognition, these technologies pave the way for more consistent, accessible, and scientifically validated TCM diagnostics.
AI Tongue Diagnosis
In Traditional Chinese Medicine (TCM), tongue diagnosis is a foundational diagnostic technique used to assess the state of the internal organs and the flow of the body’s fundamental substances—Qi (vital energy), Xue (blood), and Jin-ye (body fluids). The tongue is regarded as a mirror of the internal body, reflecting both physiological balance and pathological disturbances. Practitioners observe a range of tongue features to gather diagnostic clues, including:
-
Colour (e.g., pale, red, purple)
-
Size and shape (e.g., swollen, thin, scalloped edges)
-
Coating (e.g., thick, thin, white, yellow)
-
Moisture, texture, movement, and the presence of cracks or teeth marks
Each area of the tongue corresponds to specific organ systems—for example, the tip reflects the Heart and Lung, the sides represent the Liver and Gallbladder, the centre is linked to the Spleen and Stomach, and the root corresponds to the Kidneys and Bladder. Despite its value, tongue diagnosis is inherently subjective, relying heavily on the practitioner's experience, training, perceptual skill, and consistent lighting and viewing conditions. These challenges make standardising or replicating diagnostic outcomes difficult, creating a natural opening for technological intervention.
This growing need for objectivity and consistency has led to the emergence of AI-assisted tongue diagnosis systems, which aim to automate the analysis of tongue features using computer vision, image processing, and machine learning. The following section explores the current landscape of these technologies, including key apps and platforms, their capabilities, and the challenges they aim to overcome.

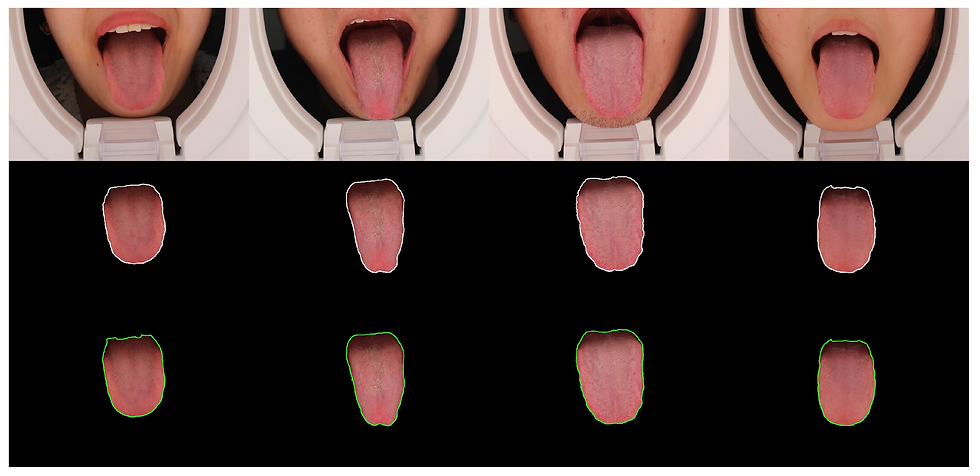
Automatic Tongue System
With the rapid evolution of artificial intelligence and computer vision, automatic tongue reading systems are beginning to reshape Traditional Chinese Medicine (TCM) diagnoses. These systems aim to automate the interpretation of tongue features by detecting patterns associated with internal imbalances in Qi, blood, and organ systems, making the diagnostic process more consistent, accessible, and potentially more accurate.
The Automatic Tongue System is a computer-aided tool that interprets digital images of the tongue according to established TCM principles. It assesses key visual elements—such as colour, coating, moisture, shape, and texture—and uses machine learning algorithms to relate these features to specific TCM syndromes. Central to this system are convolutional neural networks (CNNs), which enable the AI to process complex visual data with growing precision.
Despite being a relatively young field, several AI-powered tongue diagnosis systems and apps are already available or under development, each with varying levels of sophistication and clinical relevance. Below are a few notable examples:
Offers AI-assisted tongue diagnosis via smartphone image uploads. It analyses tongue colour, shape, coating, and texture to suggest possible TCM syndromes.
1
Uses AI and computer vision to analyse tongue images and generate health reports based on TCM diagnosis models.
Tongue Wisdom (MyZenCheck, Singapore)
2
Provides free tongue image analysis through a guided upload process, producing a visual diagnostic map with interpretations tied to TCM principles.
2
TongueMobile is a mobile application designed for the general public to perform tongue diagnosis using their smartphones. The app captures tongue images, segments the tongue body using Mask R-CNN, and classifies the tongue coating colour using deep learning models.
TongueMobile (Research Prototype)
4
Integrates AI for the "Four Diagnostic Methods"—including tongue inspection—as part of a holistic TCM diagnostic tool
BianQue AI System (China Academy of TCM)
5
This system combines deep learning with TCM to enhance the accuracy and objectivity of tongue diagnosis. It includes a hardware device for stable image acquisition, a semi-supervised learning segmentation algorithm based on U2Net, a high-performance colour correction module, and a tongue image analysis algorithm that fuses different features according to the characteristics of each TCM tongue image
Deep Learning-Based Automated Tongue Analysis System
6
This system integrates tongue detection, segmentation, and classification models into a smartphone application. It allows users to capture tongue images, which are then processed to provide diagnostic reports and treatment recommendations based on TCM principles.
7
Dr. Tongue is a framework designed for remote medical assessments, especially pertinent during the COVID-19 pandemic. It utilizes a Sign-Oriented Network (SignNet) to identify specific tongue attributes, emulating the diagnostic process of experienced practitioners.
8
TongueSAM leverages the Segment Anything Model (SAM) to perform zero-shot tongue segmentation, enabling it to handle diverse tongue images without the need for extensive labelled datasets.
9
Despite growing interest and promising developments, current tongue reading systems face several technical and practical limitations. As Matos et al. (2021) point out, several barriers still need to be addressed before these systems can be fully standardised and widely trusted. Among the most pressing challenges are:
-
Environmental lighting conditions: Variations in ambient light significantly affect image consistency. Reliable diagnosis requires controlled or standardised lighting, ideally using artificial illumination with stable temperature and intensity.
-
Low image resolution: Many mobile-based systems use standard smartphone cameras, often lacking the resolution to capture fine tongue features. This limits the accuracy of visual assessments, particularly for small signs like cracks, red spots, or subtle coating changes.
-
Lack of colour correction: Without calibrated colour systems, it becomes difficult to determine whether a tongue’s hue reflects a true physiological state or results from lighting distortion or device bias.
-
Weak correlation with clinical diagnosis: Many apps on the market currently lack robust links between their AI-generated outputs and established TCM diagnostic criteria. Until stronger clinical validation is achieved, these tools must be considered supplementary rather than definitive.
Still, the field is moving forward. Further research into AI-assisted tongue diagnostics is expected to resolve many of these issues, particularly as datasets grow in quality and diversity and image capture methods become more controlled. Addressing these design flaws, especially around imaging conditions, diagnostic accuracy, and integration with practitioner-based decision-making, will be crucial to building technically reliable and clinically meaningful systems.
Ultimately, while the Automatic Tongue System is still in development, its potential to reduce subjectivity, improve accessibility, and contribute to the standardisation of TCM practice is significant. As researchers refine the technology, these systems may soon become a trusted part of professional diagnostics and digital self-care.

The rapid advancement of smartphone technology has opened new possibilities for immediate and accessible diagnostic tools in Traditional Chinese Medicine (TCM). Among these innovations, tongue reading apps have emerged as a growing area of interest, aiming to digitise and democratise one of TCM’s core diagnostic methods. These applications typically use a smartphone camera to capture images of the tongue, which are then analysed—either manually or via AI algorithms—to infer underlying imbalances or syndromes.
Several tongue diagnosis apps are available on the market, offering various features and differing levels of accuracy, objectivity, and clinical relevance. Some rely on manual input and simple symptom mapping, while others integrate advanced image processing and artificial intelligence to assess the tongue’s shape, colour, coating, and texture in real time. These tools hold promise for self-monitoring, preventive care, and remote consultations, potentially extending the reach of TCM to broader populations. Tongue reading apps on the market include:
Tongue Reading Apps
-
AI-powered tongue diagnosis using Microsoft’s Custom Vision and Azure Medical AI Agent.
-
Provides personalised health reports based on TCM principles.
-
Secure data encryption and progress tracking.
Tongue Wisdom by MyZenCheck
1
-
Analyses tongue images to offer food and lifestyle advice based on TCM.
-
Includes a questionnaire for additional health assessment.
-
Provides warnings about potential physical and mental weaknesses.
iTongue
2
-
Educational tool for TCM students and practitioners.
-
Includes quizzes and summary theories for quick review.
-
Offline access with structured, academic references.
Tongue Diagnosis by Nguyen Tran
2
4
Qi Health
-
Offers free tongue diagnosis with holistic treatment recommendations.
-
Analyses tongue's colour, coating, shape, moisture, and texture.
-
Provides insights into overall health and potential imbalances.
5
TongueMobile
-
Automated tongue segmentation and diagnosis using deep learning.
-
Utilises Mask R-CNN for image segmentation and ResNeXt for coating colour classification.
-
Provides users with segmented images and diagnosis results.
However, significant technical and clinical challenges remain despite the enthusiasm surrounding these tools. As Matos et al. (2021) highlight, many current tongue-reading apps face limitations that hinder diagnostic reliability and clinical adoption. These include:
-
Variability in environmental lighting conditions affects colour perception and consistency.
-
There is a lack of standardised artificial illumination with controlled temperature for image capture.
-
Low image resolution on some devices reduces the ability to detect fine details critical to diagnosis.
-
The absence of reliable colour correction algorithms leads to hue and coating analysis inaccuracies.
-
A weak or inconsistent correlation between app-generated results and established clinical diagnoses reduces trust among practitioners.
These challenges highlight the need for further research and development in AI-assisted tongue diagnostics. Key areas of focus include the creation of standardised imaging protocols, improving colour and texture calibration techniques, and integrating validated diagnostic models. Furthermore, training AI systems on large, diverse datasets—paired with expert-verified annotations—will be essential for improving diagnostic precision and building clinical credibility. Future Directions include:
-
Development of smartphone attachments or controlled-light environments to improve image consistency.
-
Cross-platform data harmonisation to ensure reproducibility across devices.
-
Incorporation of user-friendly interfaces that guide proper image capture and flag poor image quality.
-
Clinical validation studies to align AI interpretations with practitioner insights and patient outcomes.
Tongue-reading apps represent a significant step forward in the digital transformation of TCM diagnostics. While current offerings show promise, they remain limited by technical constraints and a lack of clinical standardisation. Ongoing research, improved design standards, and robust AI training will be crucial to overcoming these limitations. As technology matures, these apps may evolve into highly accurate, accessible, and clinically accepted tools, bridging traditional wisdom with modern healthcare delivery.




The Future of Tongue Reading
The future of AI in Traditional Chinese Medicine (TCM) holds transformative potential, particularly in tongue diagnosis, one of the oldest and most visually rich diagnostic tools in TCM. As research and technology advance, AI is poised to reinterpret this traditional practice through highly sophisticated and objective methodologies. One of the most promising directions is the development of AI algorithms capable of analysing tongue features, such as shape, colour, coating, moisture, and fissures, with consistency and precision that surpasses human perception. By training machine learning models on large, high-quality image datasets, researchers aim to uncover subtle patterns and diagnostic markers that may not be easily discernible by even the most experienced clinicians.
While this goal has not yet been fully realised, the integration of cutting-edge image recognition systems, computer vision, and deep learning techniques makes the standardisation of tongue diagnosis increasingly feasible. Matos et al. (2021) suggest that advancements in imaging systems, combined with robust data analytics, offer a clear pathway to creating objective,
reproducible, and quantifiable tongue assessments. These technological strides could eventually lead to the parameterisation of visual indicators, laying the groundwork for digital tongue analysis to be accepted in clinical and research settings globally. Key Innovations on the Horizon include:
-
High-Resolution Imaging Systems: Enhanced optical and spectral imaging can capture nuanced tongue features under standardised conditions, improving accuracy across different lighting and skin tones.
-
AI-Powered Diagnostic Engines: Deep learning models trained on large-scale, annotated tongue image databases can link visual characteristics to syndromes, organ imbalances, and disease risk with growing accuracy.
-
Mobile Tongue Scanning Tools: With the rise of smartphones and health apps, portable AI-driven tongue reading systems can empower self-assessment and remote consultations, expanding TCM access.
-
Multimodal Integration: Combining tongue analysis with facial recognition, voice analysis, and pulse data may lead to holistic AI diagnostics that reflect the full spectrum of TCM’s four traditional methods.
The implications are vast. AI could help standardise tongue reading, reducing practitioner subjectivity and regional variation. It may also play a role in early disease detection, where minute changes in the tongue's appearance—imperceptible to the naked eye—could signal developing imbalances. In research contexts, AI could help validate TCM syndromes and establish stronger correlations between tongue features and biomedical markers.
Despite this promise, challenges remain. Standardising tongue image capture across devices, defining universal diagnostic criteria, and ensuring models generalise across populations are ongoing hurdles. Moreover, ethical concerns about data privacy and medical liability must be addressed as AI takes on more diagnostic responsibility.
The future of tongue reading lies in a fusion of ancient wisdom and advanced analytics. As AI technologies evolve, tongue diagnosis may shift from a primarily intuitive art to a rigorous, data-driven science, enhancing clinical outcomes, advancing TCM research, and promoting its integration with global health systems. With continued interdisciplinary collaboration, what once seemed a subjective craft may soon become a cornerstone of AI-enhanced precision medicine.
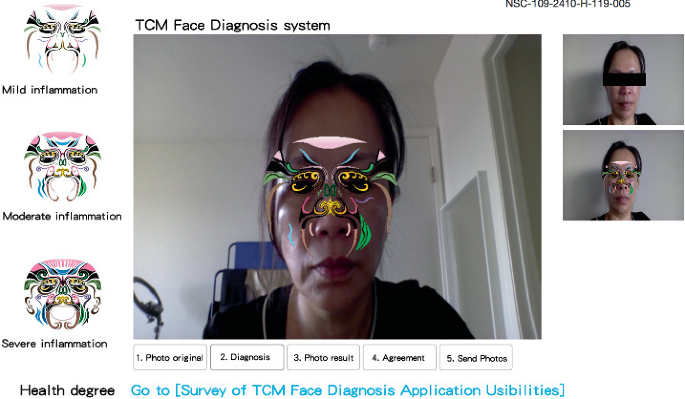
AI Facial Reading
Face reading, also known as mien shiang (面相), is an ancient diagnostic method in Traditional Chinese Medicine (TCM) that involves observing a person’s facial features to assess their health, temperament, and internal organ function. Based on the principle that the face reflects the body's internal state, this practice interprets subtle skin tone, texture, shape, and expression cues to detect physiological and pathological changes. In TCM, different regions of the face correspond to different internal organs:
-
Forehead: Heart and Small Intestine
-
Eyebrows and temples: Liver and Gallbladder
-
Nose: Spleen and Stomach
-
Cheeks: Lungs
-
Chin and jaw: Kidneys and Bladder
-
Eyes and surrounding area: Overall vitality, Shen (spirit), and blood quality
Practitioners examine a range of features, including complexion and colour tone (e.g., red, pale, greenish tint), skin texture and moisture, lines, swelling, puffiness, or sagging, asymmetry, tension, or hollowing and emotional expression and the brightness or dullness of the eyes. Face reading is particularly valued for its ability to detect latent imbalances that may not yet have manifested as physical symptoms. Like tongue and pulse diagnosis, however, it depends heavily on the practitioner’s experience, observational skill, and intuition. It can be affected by external variables such as lighting, stress, or cosmetic alterations.


AI and the Evolution of TCM Face Reading
Integrating artificial intelligence (AI) and computer vision into face reading rapidly redefines the field, offering a path to standardisation, precision, and widespread accessibility. AI-assisted face reading uses image recognition algorithms trained on thousands of annotated facial images to detect and interpret features linked to TCM diagnostic principles. Key developments include:
-
Facial zone mapping: Segmenting the face into organ-related regions for detailed analysis.
-
Skin tone and hue analysis: Objectively measuring subtle colour changes associated with blood flow, Qi stagnation, or organ deficiency.
-
3D facial modelling: Capturing fine details such as puffiness, hollowness, swelling, and symmetry changes from multiple angles.
-
Emotion and Shen recognition: Analysing micro-expressions and eye brightness to evaluate emotional and spiritual well-being (Shen).
Advanced systems are beginning to link these facial indicators to personalised diagnostic suggestions, TCM syndromes, or lifestyle recommendations. These AI models often work with other diagnostic tools (e.g., tongue analysis, pulse sensors), creating a multimodal diagnostic ecosystem that mirrors TCM's holistic nature.
About Our Business
AI has the potential to revolutionise TCM face reading in several important ways:
-
Standardisation: Removes practitioner bias and variability using measurable, reproducible image data.
-
Accessibility: Makes facial diagnostics available through smartphone apps or telehealth platforms, expanding reach to rural or underserved areas.
-
Preventive health: It enables the early detection of internal imbalances through subtle facial signs, supporting a shift from reactive to preventive care.
-
Education and training: Provides guided, data-driven feedback to assist TCM students and new practitioners in learning face reading.
-
Integration with digital health: Face reading has the potential to be included in comprehensive AI wellness platforms alongside heart rate variability, pulse diagnosis, and biometric monitoring.
However, challenges remain, including the need for large, ethnically diverse datasets, standardised image capture protocols, and clinical validation of AI-generated assessments. Additionally, preserving the human element of Shen observation—a practitioner has a sense of the spirit or vitality of the patient—remains a unique and irreplaceable aspect of TCM face reading.
AI is not replacing face reading in TCM but refining and expanding its potential. By combining ancient diagnostic wisdom with the analytical power of modern technology, AI-assisted face reading may soon become a valuable tool in professional practice and personalised wellness. As this field matures, it promises to honour the depth of TCM traditions while ushering in a new era of data-driven, accessible, and preventative medicine.

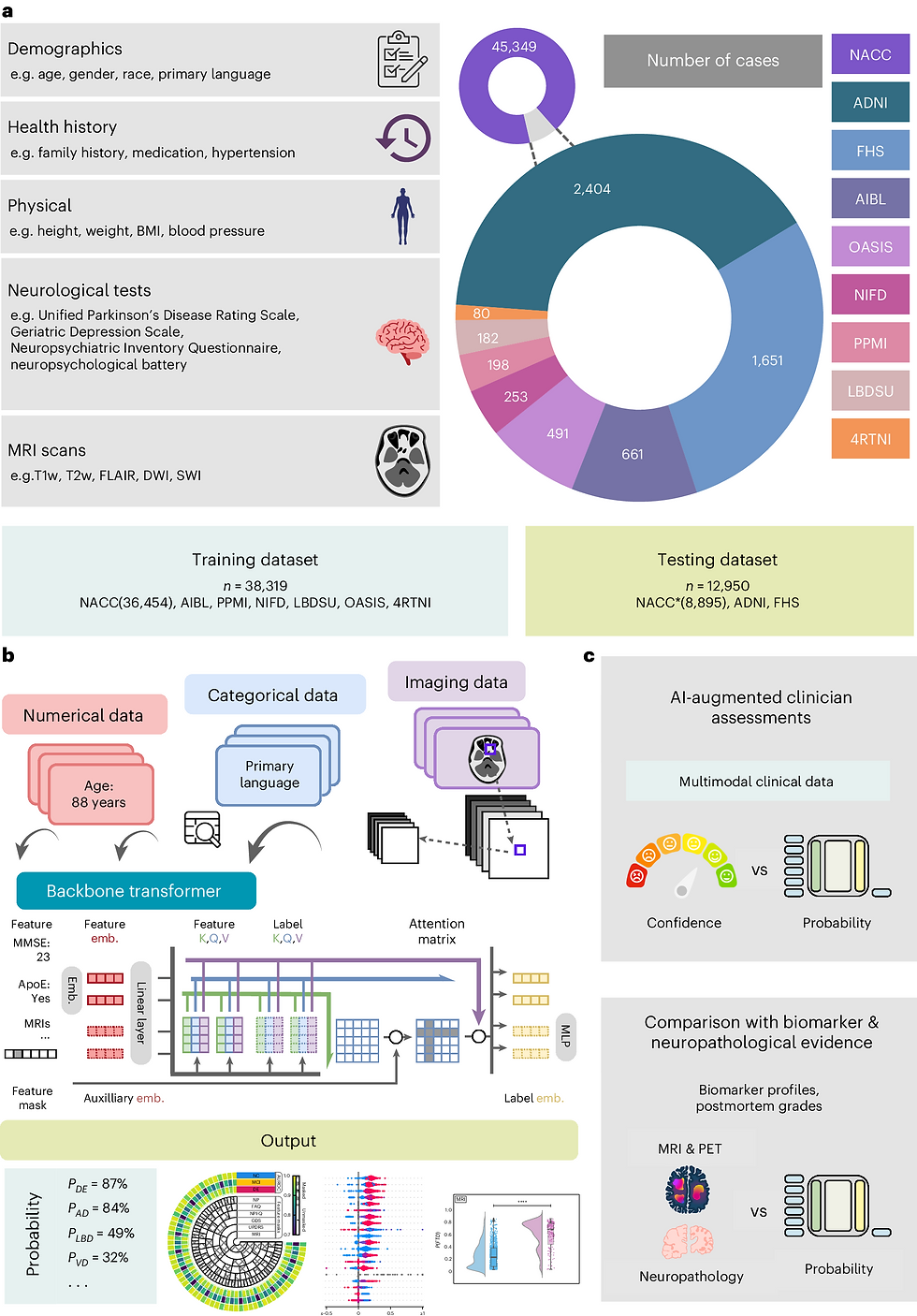
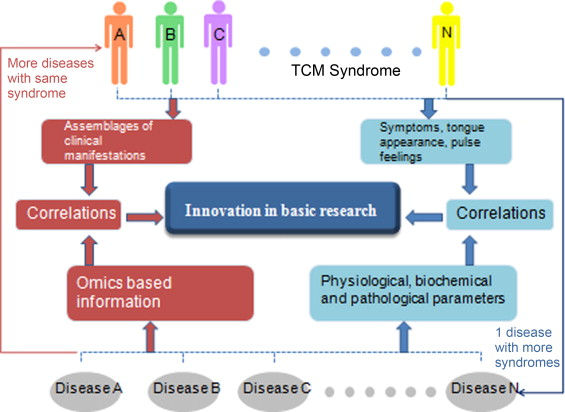

AI And Syndrome Differentiation
Syndrome differentiation (辨证论治, bian zheng lun zhi) lies at the heart of Traditional Chinese Medicine (TCM). It is the central diagnostic principle through which practitioners analyse symptoms, tongue and pulse features, and constitution to determine a patient’s syndrome—an integrated picture of physiological and pathological changes. Syndrome differentiation distinguishes between diseases (病, bing) and the syndromes (证, zheng) that reflect the patient's internal imbalances in Qi, blood, Yin-Yang, and organ function. The process is inherently holistic and interpretive, requiring years of clinical training. However, it can be highly subjective and variable between practitioners. Artificial Intelligence (AI) offers a breakthrough opportunity to bring greater accuracy, consistency, and objectivity to syndrome differentiation by analysing large, complex datasets that traditional methods cannot easily process.
Modern AI models—particularly Bidirectional Long Short-Term Memory with Conditional Random Fields (BiLSTM-CRF) and Transformer architectures—are now being trained to emulate and enhance human reasoning in syndrome classification:
-
BiLSTM-CRF models are well-suited to processing sequential patient data, such as symptom descriptions, case histories, and pulse/tongue image features. They can learn temporal dependencies and contextual relationships, improving classification accuracy overrule-based systems.
-
Transformer models—especially those adapted from NLP tasks—excel at understanding complex patterns across large text and image datasets. They can simultaneously process multimodal information (e.g., symptoms + tongue + pulse), offering a comprehensive analysis of patient data.
These models are trained using annotated medical records and expert-labelled datasets, allowing them to learn the implicit logic of TCM diagnosis and provide exceptionally reliable syndrome predictions.
AI-enhanced syndrome differentiation directly impacts individualised treatment strategies, a foundational principle in TCM. With precise syndrome classification, AI can support practitioners in selecting the most appropriate herbs, acupuncture points, or therapeutic approaches. This is particularly valuable in chronic disease management and cancer care, where accurate syndrome diagnosis must be matched with herbal formulations tailored to the patient's internal environment.
Some systems go a step further by linking syndrome patterns to chemical composition data of herbs and patient biomarkers. This enables AI to recommend herbal prescriptions based on energetic and biochemical compatibility, bridging the gap between traditional theory and modern pharmacological insight. Integrating AI into syndrome differentiation offers several important benefits:
-
Standardisation: Reduces diagnostic variability across practitioners and institutions
-
Efficiency: Shortens the time required for complex diagnostic reasoning
-
Clinical Support: Offers second opinions or confirmations to assist less experienced clinicians.
-
Scalability: Makes TCM diagnostic logic accessible in remote or underserved areas via mobile platforms
-
Research Advancement: Supports retrospective analysis, syndrome pattern discovery, and integration with Western medical data.
AI-driven syndrome differentiation represents a critical frontier in modernising Traditional Chinese Medicine. By enhancing the accuracy and objectivity of core diagnostic processes, AI supports clinicians in delivering personalised care and reinforces TCM's scientific foundation. As AI models become more sophisticated and datasets more comprehensive, we are moving toward a future where ancient diagnostic wisdom is augmented by powerful computational tools, opening new pathways for integrative, precise, and globally credible TCM practice.
The Future of Data Collection
As Traditional Chinese Medicine (TCM) enters the digital age, data collection and interpretation are becoming increasingly central to clinical care and research. AI technologies, particularly deep learning and neural networks, are poised to revolutionise how data is gathered, processed, and applied within the TCM framework. AI excels at interpreting complex, multi-layered information typically collected during a TCM consultation—including symptoms, tongue and pulse observations, lifestyle patterns, and constitutional characteristics. Deep learning algorithms can analyse high-dimensional patient data, identifying subtle patterns that may elude human practitioners. Data mining techniques enhance this capacity by uncovering hidden relationships within real-world prescription data, offering valuable insights into syndrome-treatment correlations and evolving clinical practices (Li et al., 2024).
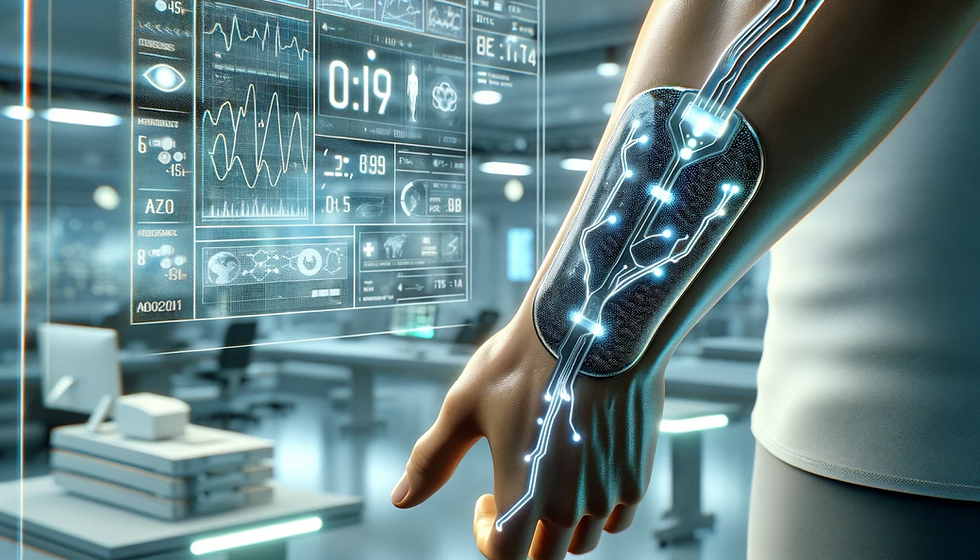
AI provides a powerful tool for tracking disease progression and predicting relapses for patients with chronic illnesses. By analysing longitudinal data from electronic health records (EHRs), AI can generate predictive models that assist practitioners in making more precise, data-informed diagnoses. Furthermore, AI can support personalised lifestyle guidance by offering tailored diet, exercise, and self-care recommendations, significantly improving patients’ quality of life while reducing the risk of relapse. These capabilities are enhanced by the rise of smart wearables, which allow for real-time health monitoring. These devices collect continuous biometric data, such as heart rate, sleep patterns, stress levels, and physical activity, which is transmitted directly to AI systems for analysis. This real-time feedback loop enables early detection of emerging health concerns. It allows patients and practitioners to take proactive, preventive action, making AI integral to ongoing care and wellness maintenance within TCM.
AI offers transformative possibilities for TCM by making data collection more dynamic, intelligent, and precise. AI tools are creating a new paradigm for personalised, preventative care, from wearable technologies to language-based diagnostic assistants. While integrating AI into the TCM diagnostic process presents challenges, particularly around the alignment of knowledge systems, it also holds the promise of a modernised yet faithful evolution of TCM. By embracing these technologies thoughtfully and collaboratively, the TCM community can harness AI to enhance diagnosis, expand access, and deepen its contributions to global health in the 21st century.


The Future Medical Diagnostics in TCM
Integrating Artificial Intelligence (AI) with Traditional Chinese Medicine (TCM) diagnostics is reshaping the future of medical diagnosis. By merging classical diagnostic principles with advanced computational methods, this fusion enhances the interpretation of chemical components and their correlation with clinical symptoms, the analysis of complex symptom patterns and the prediction of disease trajectories and the overall efficiency, accuracy, and objectivity of diagnostic outcomes.
This synergistic approach enables a deeper, data-driven understanding of the intricate relationships between chemical constituents, syndrome differentiation, and specific disease manifestations, providing a more refined and personalised diagnostic model rooted in TCM principles.
Contemporary TCM research increasingly recognises the diagnostic significance of bioactive chemical components found in herbs, bodily fluids, and pathological markers. These components are potential biomarkers for identifying diseases and therapeutic targets, offering a biochemical dimension to traditionally energetic concepts such as Qi stagnation, heat toxins, or blood deficiency. However, the chemical complexity of TCM formulations and the multifactorial nature of disease patterns present significant analytical challenges. Conventional tools often fail to uncover the nonlinear and multivariate interactions between chemical profiles and syndromic expressions.
AI addresses these challenges through machine learning, deep learning, and pattern recognition algorithms that can sift through large volumes of high-dimensional data to identify meaningful trends. These technologies:
-
Process and categorise chemical compound data related to herbs and human physiology.
-
Detect subtle, non-obvious correlations between symptoms, biochemical changes, and disease types.
-
Support disease classification and syndrome differentiation with higher granularity and accuracy.
-
Aid in the discovery of novel diagnostic markers and compound synergies within herbal prescriptions.
For example, deep learning models can be trained on annotated datasets to predict disease progression by analysing dynamic chemical signatures, contributing to early diagnosis and proactive risk management.
Beyond reactive diagnosis, AI’s predictive capabilities open the door to proactive, preventative care. By continuously analysing patient data—including symptoms, chemical markers, and historical trends—AI can forecast disease development, stratify patient risk, and recommend personalised interventions before the condition worsens. This represents a shift from episodic, symptom-based care to continuous health monitoring and predictive intervention, aligning closely with TCM’s focus on balance, harmony, and disease prevention.
The fusion of AI with TCM diagnostics marks a significant leap in the evolution of personalised medicine. By interpreting chemical data and integrating machine learning models, this approach enhances diagnostic accuracy and reproducibility, clinical efficiency, practitioner decision-making, patient-specific treatment strategies and long-term health outcomes. By leveraging the power of AI and the rich, structured datasets found in TCM databases, the medical community can advance toward a future where cutting-edge technologies augment TCM’s holistic wisdom. This convergence validates, modernises traditional practices, and offers a new paradigm of precise, integrative, and intelligent healthcare.

The Future of TCM Diagnostics
The future of Traditional Chinese Medicine (TCM) diagnosis lies in the seamless integration of artificial intelligence (AI) and advanced technologies to enhance diagnostic practices' accuracy, objectivity, and efficiency, while honouring and preserving TCM’s holistic principles. This evolution envisions a hybrid diagnostic system that draws on both traditional knowledge and cutting-edge tools, with key developments including:
-
AI-Powered Diagnostic Tools: Intelligent systems for tongue, pulse, facial, and olfactory diagnostics are being developed to objectify and standardise the four traditional TCM diagnostic methods: inspection, listening/smelling, inquiry, and palpation. These tools can support clinical accuracy and reproducibility while enhancing diagnostic speed.
-
Smart Diagnostic Devices: AI-enabled devices using sensors, computer vision, and pattern recognition can objectively interpret TCM cues, such as pulse qualities, tongue coatings, facial features, and vocal tones, mirroring the observations of experienced practitioners.
-
Advanced Data Analytics: Machine learning and deep learning algorithms can be applied to large, diverse TCM clinical datasets to identify syndrome patterns, predict treatment efficacy, and personalise care strategies based on patient constitution and disease progression.
-
Holistic AI Models: Future AI systems will be trained to incorporate TCM’s holistic worldview, evaluating interconnected physiological, emotional, and environmental factors to provide comprehensive health assessments and tailored treatment suggestions.
-
Chinmedomics: This emerging discipline integrates TCM with omics technologies (e.g., genomics, metabolomics) to identify the molecular basis of TCM syndromes and herbal effects. Chinmedomics can help validate traditional diagnostic categories and refine precision treatments.
-
Molecular Profiling: Techniques that analyse blood, urine, and stool samples at the molecular level offer objective biomarkers to complement subjective TCM diagnostics, further bridging traditional insight with modern clinical standards.
Recent advancements highlight the transformative role of AI in TCM diagnostic techniques. Recent advancements include image Recognition for standardised tongue and facial diagnosis, Sensor Technology and audio analysis algorithms for objective auscultation, Olfactory AI algorithms using odour mapping and biomarker identification for smell-based diagnostics, tactile pulse measurement devices for consistent and replicable pulse analysis, deep learning systems for nuanced symptom assessment and algorithmic support for refining and individualising treatment protocols. For these innovations to reach full potential, future efforts should focus on:
-
Developing high-precision sensors to improve data reliability for sound, odour, pulse, and visual characteristics
-
Training AI models on diverse, high-quality datasets to identify subtle and complex health patterns.
-
Ensuring cross-device algorithm compatibility, enabling AI to analyse data from multiple hardware platforms with consistent results
-
-
Promoting interoperability between data systems to facilitate multi-centre research and collaborative diagnostics
The future of TCM diagnosis will not be a departure from tradition but an expansion of it. By integrating AI-driven precision with the wisdom of holistic observation, we are entering a new era where diagnosis becomes more accurate, replicable, and accessible. This convergence offers a vision of intelligent, compassionate, and integrative healthcare, rooted in the past but empowered by the future.
Objectifying TCM Diagnosis
Objectifying Traditional Chinese Medicine (TCM) diagnosis refers to using objective, technology-driven methods to assess a patient's condition, shifting away from subjective interpretations traditionally based on practitioner experience. This transformation aims to bring greater accuracy, consistency, and scientific rigour to TCM by integrating digital tools, data analytics, and algorithmic modelling. Core Components of Objectified TCM Diagnosis include:
-
Digital Tongue Diagnosis: Image processing and computer vision techniques are employed to analyse the tongue's colour, shape, texture, and coating. These features, which in TCM reflect organ health and internal imbalances, are now being quantitatively assessed using AI-powered tongue image analysis platforms.
-
Pulse Waveform Analysis: Traditional pulse diagnosis, once reliant on a practitioner’s touch and interpretation, is now being modernised through electronic sensors. These tools measure pulse depth, rhythm, intensity, and waveform to detect subtle physiological variations, transforming subjective impressions into measurable physiological data.
-
Machine Learning and Data Analysis: AI algorithms are being trained on vast datasets of TCM diagnostic information—including symptoms, signs, and treatment outcomes—to identify patterns, correlations, and diagnostic models. These computational tools support more precise syndrome differentiation and inform personalised treatment planning.
By relying on quantifiable data rather than practitioner intuition alone, objectification enhances the reliability and reproducibility of TCM diagnostics. Digital tools can detect subtle features and correlations often missed by the human eye or touch, supporting earlier and more accurate diagnosis. Objective data allows for standardising diagnostic protocols, enabling meaningful comparisons across clinical studies and facilitating scientific validation of TCM practices. Objectified diagnostic data can be easily shared among practitioners, researchers, and institutions, promoting greater collaboration and knowledge exchange. Despite the promise of objectification, several challenges remain:
-
Complexity of TCM Theory: TCM relies on dynamic, holistic frameworks, such as Yin-Yang, the Five Elements, and Qi flow, which are difficult to reduce into discrete variables without oversimplifying the system.
-
Lack of Standardised Terminology and Protocols: Variability in how symptoms and syndromes are described across TCM schools complicates the development of unified objectification models.
-
Need for Further Research and Validation: While progress has been made, more rigorous clinical trials and algorithm training are needed to ensure that objectified tools reflect authentic TCM principles and yield accurate results.
The objectification of TCM diagnosis marks a pivotal step in the evolution of Chinese medicine in the digital age. By combining ancient wisdom with modern scientific methods, objectification enhances diagnostic accuracy, facilitates research, and strengthens communication among practitioners, without losing sight of TCM’s holistic philosophy. Ongoing investment in technology, interdisciplinary collaboration, and clinical validation will be essential to refine these tools and ensure that the spirit of TCM is preserved even as its methods are modernised. In doing so, TCM can offer a harmonised model of care that bridges tradition and innovation to benefit global health.

The Integrated TCM Platform
An Integrated TCM Diagnostic Platform represents a transformative step in the future of Traditional Chinese Medicine—uniting the depth of ancient diagnostic wisdom with the precision of digital technologies. These platforms enhance diagnostic accuracy, efficiency, standardisation, and collaborative knowledge-sharing among practitioners, researchers, and patients. Key Features of an Integrated TCM Diagnostic Platform include:
-
Holistic Diagnostic Framework: True to TCM's holistic philosophy, integrated platforms synthesise information from diverse diagnostic sources—including pulse, tongue, facial features, vocal tones, symptoms, and lifestyle factors—to provide a comprehensive understanding of the patient’s physical and energetic state.
-
Advanced Digital Tools: Leveraging artificial intelligence (AI), machine learning, and data analytics, these platforms can collect, process, and interpret a wide range of clinical data. AI-driven image recognition technologies can analyse tongue and facial images, while sensor arrays and signal processing algorithms can objectify pulse, sound, and olfactory diagnostics.
-
Personalised Treatment Recommendations: Based on an individual’s diagnostic profile, the platform can generate tailored treatment plans, suggesting herbal formulations, acupuncture points, dietary advice, and lifestyle modifications. These personalised protocols aim to restore internal balance and address the root cause of disharmony, which is central to TCM's therapeutic model.
-
Automation for Practitioner Support: Repetitive and time-consuming tasks, such as image analysis, symptom classification, or initial treatment recommendations, can be automated, allowing practitioners to dedicate more time to patient interaction, clinical reasoning, and therapeutic strategy.
-
Collaborative Knowledge Sharing: By standardising and digitising diagnostic data, integrated platforms facilitate real-time collaboration and knowledge exchange between practitioners, improving continuity of care and fostering interdisciplinary learning.
To realise the full potential of an integrated TCM diagnostic platform, several developmental challenges must be addressed:
-
Standardisation and Interoperability: Establishing unified data collection standards, terminology, and diagnostic criteria is a critical step. Harmonising these standards across devices and systems enables consistent data interpretation and supports large-scale collaborative research.
-
Multimodal Data Integration: Future platforms must refine the ability to synchronise diverse forms of diagnostic data—pulse signals, tongue images, voice recordings, odour profiles—into coherent diagnostic outputs that align with TCM syndrome differentiation frameworks.
-
AI Model Training and Validation: Using machine learning and classification techniques, large, annotated datasets must be collected to train AI models capable of accurately recognising and categorising TCM syndromes. This includes extensive data on pulse patterns, tongue characteristics, facial expressions, and more.
-
Quantification and Benchmarking: The development of quantifiable metrics and performance benchmarks is essential for evaluating AI diagnostic accuracy, tracking progress, and guiding further innovation. These benchmarks also support regulatory approval and clinical acceptance of AI-assisted diagnostic tools.
The Integrated TCM Diagnostic Platform represents a bold vision for the future—objectifying ancient techniques, digitising practitioner wisdom, and unifying diagnostic practices within a seamless technological framework. By combining centuries-old knowledge with AI's analytical power, we can create a next-generation diagnostic system that is precise, scalable, and personalised, while remaining deeply rooted in the foundational principles of Traditional Chinese Medicine.